For decades, multiple sclerosis (MS) has been somewhat of a black box, with no way to know why the disease progresses in some people but not others, and which treatments will stop it in its tracks. But a new global data sharing platform that leverages the extraordinary powers of artificial intelligence is about to unlock some of those mysteries.
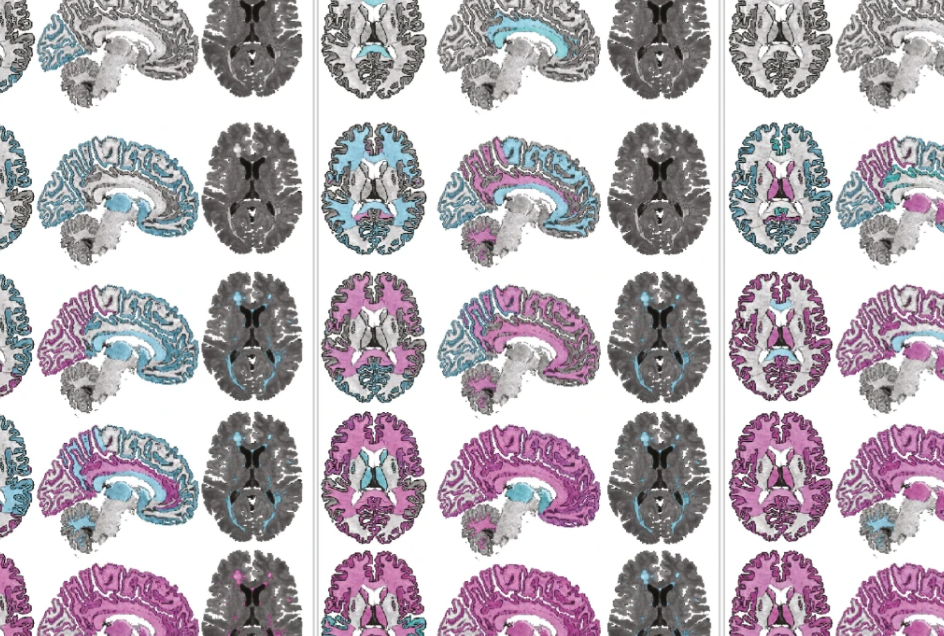
The new MS Clinical and Imaging Data Resource (CIDR) was created as an outcome of work supported by the International Progressive MS Alliance (Alliance). This new platform — which builds on previous Alliance investments in creating an Imaging and Clinical Trials Collaborative Research Network — brings together anonymized information from over 13,500 people affected by progressive MS and includes more than 72K MRI scans and clinical data from 200K+ clinical visits collected as part of high-quality clinical trials.
Most remarkably, all of this data, which was collected using diverse methods and donated by different pharmaceutical companies, has been “harmonized,” or standardized, so that MS scientists and companies around the world could submit research proposals to access and analyze data using state-of-the-art tools such as artificial intelligence and machine learning, with the goal of finding patterns that humans may not have seen or considered.